

ConclusionsĪge is a major impact factor for aTAAD surgery. The postoperative morbidity of gastrointestinal bleeding and bowel ischemia were 16.7% and 11.1% in 80 s group. The overall mortality was 14.1%, the tendency of mortality was increased with age except 20 s group (33.3% in 80 s, P = 0.016). Young age groups (20–60 s) had a higher rate of root replacement and total arch replacement, which led to a longer duration of operation and hypothermic circulation arrest. Preoperative hypotension was highest in 80 s (16.7%, P = 0.038). The multiple comorbidities were more common in old age groups (60 s, 70 s, 80 s), while the 20 s group patients had the highest proportion of Marfan syndrome (28.1%).

The median age was 52.0 years old in whole cohort. During a median follow-up term of 17 months, the survival rates were compared among 7 groups through Kaplan–Meier analysis. The differences between the groups were analyzed in terms of the baseline preoperative conditions, surgical methods and postoperative outcomes of patients of different age groups.
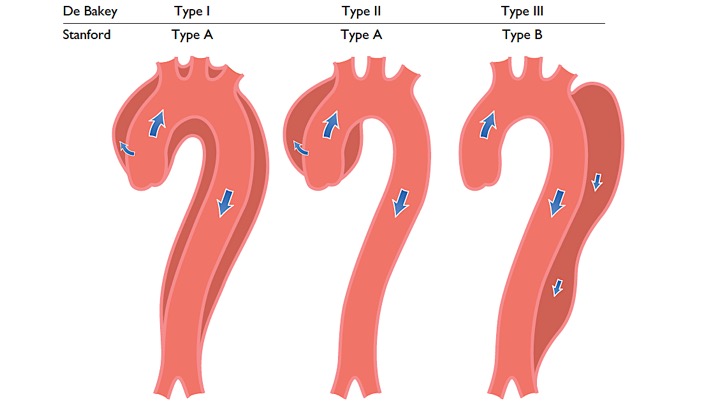
Patients were divided into 7 groups according to every ten-year interval (20–80 s). This retrospective study was to analyze the impact of age stratification in aTAAD, and to provide clues for surgeons when they make choices of therapy strategies.įrom January 2011 to December 2019, 1092 aTAAD patients from Nanjing Drum Tower Hospital received surgical therapy. Acute type A aortic dissection (aTAAD) is a lethal disease and age is an important risk factor for outcomes.


 0 kommentar(er)
0 kommentar(er)
